Igniting the Future of Medicine: Generative Artificial Intelligence Disrupting Medicine's Core
Generative artificial intelligence is reshaping diagnostics, treatment planning, and clinical decision support by combining language capabilities with medical domain knowledge to augment clinician workflows and improve patient care. This introduction synthesizes how Artificial intelligence and machine learning integrate with precision medicine, data analysis, and clinical decision making to reduce diagnostic delays and advance cancer detection using cancer imaging biomarkers and deep-learning applications. Practical pilots show healthcare organizations measuring faster triage and improved documentation, and many teams leverage HTTPS-secured APIs for model interoperability and patient portal messaging. For practical implementation guidelines and vendor-neutral methodologies, consult comprehensive generative AI implementation resource to ground governance and procurement decisions in evidence-based medicine. Actionable steps include defining clinical use cases, curating domain-specific datasets, validating transformer model architectures on held-out cohorts, and adopting robust validation approaches to ensure safety. Institutions should establish multidisciplinary teams with primary care physicians, data scientists, and ethicists to prioritize general practice adoption and build workflows that reduce administrative burden and support patient care innovation.
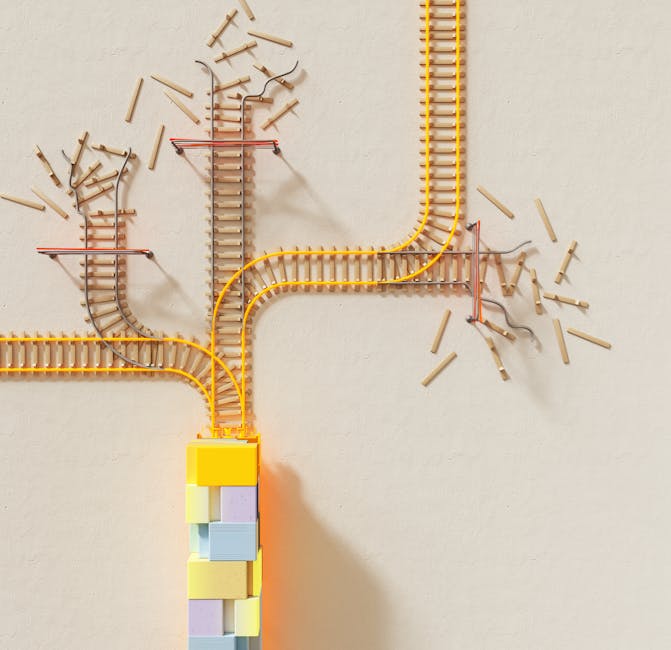
Infographic of AI pipeline showing data, model training, validation, deployment, monitoring in clinical workflows
Unveiling the Transformative Power of Artificial Intelligence in Medicine
Artificial intelligence and Artificial Intelligence-driven solutions are unlocking new diagnostics and operational efficiencies across healthcare systems, from intelligent machines aiding radiology reads to language models supporting clinical documentation and patient triage. Google-scale approaches and neural networks have shown improved sensitivity in cancer detection and cancer survivorship monitoring when combined with clinical context, and Generative artificial intelligence (GAI) tools now synthesize literature, provide decision support, and accelerate research workflows. Practical examples include Med-PaLM and ChatGPT-style prototypes adapted for evidence-based medicine, and implementations must emphasize Secure .gov or HTTPS endpoints, reproducible training, and transparent validation approaches. Organizations must prioritize medical AI safety, incorporate social determinants of health into models, and deploy domain-specific datasets to reduce bias. Actionable recommendations: conduct calibration studies, perform external validation on independent cohorts, and create clinician-facing interfaces that integrate into existing EHRs to reduce friction.
Diagram showing AI augmenting radiology, pathology, primary care, and patient portal messaging systems
Crucial AI Solutions and Key Areas Covered by Medical Artificial Intelligence
Medical artificial intelligence spans diagnostics, predictive analytics, patient triage, and workflow automation, with deep learning system components tailored for tasks like muscle mass tracking, type 1 diabetes monitoring, and oncology biomarker discovery. In practice, machine learning pipelines ingest structured EHR data, imaging, and unstructured notes, leveraging Natural Language Processing to summarize clinical encounters and support clinical decision making. AI in medicine must be evaluated across peer-reviewed venues like JAMA Network and Journal of Medical Artificial Intelligence to measure clinical impact, transparency, and reproducibility; metrics should include sensitivity, specificity, calibration, and impact on primary care physicians’ workload. Developers should use Creative Commons Attribution–licensed datasets where possible, document external validity, and design clear governance for deployment to private practice and hospital systems. Operational guidance includes continuous monitoring, retraining schedules, and involving clinicians early in design to ensure adoption.
Workflow illustration integrating EHR data, imaging, NLP, model outputs into clinician dashboard
Why Generative Artificial Intelligence in Medicine Program Matters: A Deep Dive into Patient Outcomes
Generative artificial intelligence programs are important because they can synthesize patient histories, prioritize diagnostics, and suggest personalized treatment pathways that support precision medicine and improved patient outcomes; documented reductions in time-to-diagnosis and improved documentation quality are measurable benefits. These systems combine transformer model architectures with domain-specific datasets to perform biomedical tasks such as extracting cancer imaging biomarkers and supporting clinical decision making in oncology and chronic disease management. Implementation should include clear validation approaches, external test sets, and randomized evaluations when feasible to demonstrate impact on patient triage and outcomes. Clinicians must be trained in interpreting probabilistic outputs and integrating AI prompts into general practice workflows to maintain trust and patient safety. Governance frameworks should mandate HTTPS for data exchange, involve legal review, and align with evidence-based medicine principles to support adoption.

Visual comparing outcomes before and after AI adoption in oncology clinics with annotated metrics
Laying the Groundwork: Essential Background Information on Artificial Intelligence Applications
Understanding foundational concepts of artificial intelligence is critical for safe clinical deployment: supervised, unsupervised, and reinforcement learning paradigms each have strengths for specific biomedical tasks. Developers and clinicians should prioritize reproducible pipelines, robust data provenance, and adherence to privacy-preserving practices when using patient Face Photos, muscle mass tracking data, or biological signals related to Biological Age estimations. Incorporating machine learning best practices—feature engineering, cross-validation, external validation, and bias audits—helps ensure models generalize across diverse populations. Healthcare organizations should map use cases to measurable KPIs such as reduced patient portal messaging latency, improved Match performance for trainees, or decreased administrative overhead for medical students and clinicians in training. Successful programs combine human intelligence oversight with automation to enhance clinician decision making without replacing judgement, and design considerations must include Secure .gov or HTTPS endpoints for public reporting and data access.

Background diagram showing supervised and unsupervised learning workflows applied to clinical datasets
The Current Frontier of Augmented Intelligence in Clinic Practice: Latest Updates and Challenges
Augmented intelligence blends human clinicians with AI tools to improve diagnostics, documentation, and care coordination, but the frontier is marked by challenges in validation, bias mitigation, and workflow integration. Recent studies highlight improvements in triage accuracy and efficiency, while others caution that models trained on limited domain-specific datasets may underperform in real-world settings. Implementers should run prospective validation approaches, include clinicians in iterative design sprints, and monitor outcomes such as patient care metrics and clinician satisfaction to evaluate real-world impact. A focus on automation that reduces routine clerical tasks can lower physician burnout, while continued collaboration with regulatory bodies ensures compliance. Organizations must also consider scalability, cost-benefit analysis, and evidence dissemination through channels like JAMA Network and the Journal of Medical Artificial Intelligence to build trust.
Clinic scene showing clinician reviewing AI-generated report with patient in examination room
Understanding the Fundamentals of Artificial Intelligence in Health Care
Fundamentals include probabilistic modeling, feature selection, neural networks, interpretability techniques, and deployment considerations such as secure HTTPS APIs and model monitoring. Clinicians should be literate in performance metrics, understand limitations of language models, and demand transparent reporting of training data and generalizability to diverse populations. Case studies demonstrate that calibrated models can improve diagnostics and reduce time-to-treatment, but they require ongoing evaluation against clinical outcomes like diagnostics accuracy, patient triage timeliness, and long-term follow-up in cancer survivorship. Educational programs should cover AI in medicine, Natural Language Processing for clinical notes, and human-AI interaction design to prepare primary care physicians and specialists for collaborative workflows.

Educational graphic mapping AI concepts to clinical scenarios and training modules
Deconstructing Key Concepts of Medical Artificial Intelligence: An AI Taxonomy
A clear taxonomy helps stakeholders differentiate between predictive algorithms, generative systems, and decision-support tools, specifying intended use, inputs, outputs, and risk profiles for regulators and clinicians. This taxonomy should reference transformer model architectures for generative tasks, neural networks for imaging, and hybrid models for workflows that integrate language models with clinical rules. Documenting the taxonomy supports evidence-based medicine by clarifying validation approaches, datasets used, and expectations for clinical decision making, including diagnostics and patient triage. Design teams should map taxonomy elements to monitoring plans, retraining frequency, and escalation protocols for uncertain outputs. The taxonomy further guides procurement, enabling health systems to compare vendor claims and align solutions with organizational goals for health care transformation.

Taxonomy chart categorizing predictive, generative, and diagnostic AI tools with examples
Critical Roles of AI-powered Tools in Diagnosis
AI-powered tools in diagnosis accelerate image interpretation, pattern recognition, and risk stratification, often outperforming baseline heuristics while complementing clinician expertise to improve precision medicine outcomes. In oncology, models trained on domain-specific datasets detect subtle cancer imaging biomarkers and flag high-risk lesions for expedited review, improving cancer detection and potentially survival. Implementation requires rigorous external validation, calibration studies, and transparent reporting in line with JAMA Network expectations and Journal of Medical Artificial Intelligence standards to ensure reproducibility. Clinicians should understand model limitations, maintain human oversight, and use AI outputs as one component of broader evidence-based medicine. Operationally, integrate outputs into EHR workflows, secure HTTPS endpoints for model inference, and monitor impact on patient care metrics and physician workload to demonstrate value.
Radiology workstation showing AI highlighting suspicious lesion and clinician annotation overlay
Identifying Important Factors for Successful AI Integration
Successful integration depends on governance, data quality, clinician engagement, technical infrastructure, and continuous evaluation; poor data governance leads to biased models and unsafe recommendations. Key factors include assembling multidisciplinary teams, ensuring high-quality labeled data, performing external validation approaches, and tracking outcomes such as patient triage efficiency and reductions in administrative burden. Investment in secure HTTPS infrastructure, interoperability standards, and training materials for clinicians enhances adoption. Additionally, organizations should measure adoption via concrete KPIs like reduced patient portal messaging backlog and improved diagnostic throughput, and communicate results through official websites and peer-reviewed publications to support transparency and continuous improvement.
Flowchart of governance, data quality, validation, and monitoring processes for AI deployment
In-Depth Analysis of Artificial Intelligence Applications in Clinic Practice
Applying AI in clinic practice spans triage prioritization, appointment scheduling optimization, and clinical decision support embedded within EHRs, delivering measurable improvements in response times and care coordination. Successful pilots often begin with focused use cases—such as automating routine documentation, flagging high-risk referrals, or predicting readmissions—using machine learning models that undergo prospective validation and clinician review. Data analysis should incorporate social determinants of health to reduce disparities and ensure models generalize across populations. Performance monitoring, retraining cadence, and clinician feedback loops are essential for sustained benefits and reduction of false positives that could burden workflows. Integration must also consider human factors design to ensure outputs assist rather than distract clinicians.

Clinic staff using tablet showing AI-driven scheduling and patient risk stratification dashboard
Pinpointing Critical Elements for Effective AI Solutions
Effective AI solutions combine clinical relevance, robust evidence, scalable architecture, and human-centered design to achieve measurable outcomes such as improved diagnostics, reduced clinic wait times, and enhanced patient triage. Teams must prioritize interoperability through HTTPS-secured APIs, maintain version control for models, and implement rigorous validation approaches including external cohorts and prospective trials where feasible. Design efforts should incorporate clinician workflows to reduce cognitive load and align with evidence-based medicine standards; for instance, leveraging language models to summarize patient histories can save time while preserving clinical nuance. Track implementation metrics—diagnostic accuracy shifts, clinician time savings, and patient satisfaction—and publish results in venues like the Journal of Medical Artificial Intelligence to inform the broader community.
Diagram showing integration of AI modules into hospital IT architecture with monitoring nodes
Adopting Best Practices for Physician-Machine Collaboration
Best practices emphasize transparent model outputs, clinician training, clear escalation pathways, and interfaces that present actionable recommendations rather than raw probabilities. Training programs for primary care physicians and specialists should include interpretation of language models, understanding of transformer model architectures, and protocols for when to override or consult human experts. Workflow pilots should measure physician burnout, Match performance for trainees, and patient care outcomes such as reduced time-to-diagnosis and improved follow-up for chronic conditions. Establishing shared mental models between clinicians and AI systems builds trust, enabling safer automation of routine tasks and better allocation of clinician time to complex decision making.
Training session image showing clinicians learning to interpret AI explanations on a projector screen
Implementing Cutting-Edge AI Solutions for Enhanced Medical Outcomes
Implementations that emphasize clinical validity, scalability, and clinician-centered design deliver enhanced outcomes: reduced diagnostic errors, streamlined triage, and improved documentation quality. Adopt robust data pipelines feeding domain-specific datasets, perform external validation, ensure HTTPS-secured inference endpoints, and define monitoring metrics for patient care and clinician workload. Include stakeholder engagement across legal, compliance, and clinical operations to address liability and patient safety questions. Use early adopter case studies to refine deployment strategies and train clinicians on interpreting generative outputs to support evidence-based medicine. Continuous quality improvement cycles help maintain model performance and adapt to evolving clinical patterns.

Deployment roadmap graphic showing stages from pilot to scale with stakeholder checkpoints
The Current Frontier of Augmented Intelligence in Clinic Practice: Latest Updates and Challenges
Deploying AI requires staged growth: pilot, validation, limited rollout, and scale, with each phase governed by predefined success metrics and quality gates that prioritize patient safety and clinician acceptance. Start with clearly scoped use cases, secure high-quality labeled data, apply machine learning best practices, and run prospective validation approaches to measure real-world impact on diagnostics, patient triage, and patient care metrics. Ensure HTTPS-secured endpoints, robust logging, and explainability mechanisms so clinicians can trust outputs, and schedule retraining based on drift detection. Engage clinical champions to shepherd adoption and collect continuous feedback to refine interfaces and thresholds. Establish governance for evidence-based medicine reporting, and publish outcomes in peer-reviewed venues to support broader adoption.

Stepwise diagram showing pilot, validation, rollout, and scale phases with KPIs and decision gates
Understanding the Fundamentals of Artificial Intelligence in Health Care
Navigating adoption involves stakeholder alignment, technical readiness assessments, pilot design, and rigorous evaluation using prospective cohorts and external validation to ensure clinical benefits. Define success in operational and clinical terms—reduced documentation time, improved diagnostics, or enhanced patient triage—and instrument systems to measure these outcomes. Secure HTTPS connections and follow security best practices for data exchange, and develop clinician-facing dashboards that present interpretable outputs and escalation pathways. Use change management tactics,education sessions, and iterative sprints to integrate tools with minimal disruption to workflows, and plan for regulatory reporting and ongoing monitoring to maintain trust.

Roadmap showing timelines, stakeholder roles, and evaluation milestones for adoption process
Deconstructing Key Concepts of Medical Artificial Intelligence: An AI Taxonomy
Common challenges include data silos, bias, clinician resistance, and regulatory uncertainty; overcoming them requires proactive governance, transparent validation approaches, and clinician engagement. Address data silos by harmonizing EHRs, curating domain-specific datasets, and implementing secure HTTPS transfer protocols. Perform bias audits, include diverse training cohorts, and validate performance across demographic subgroups to mitigate disparities. Educate clinicians on AI limitations and integrate human oversight into decision pathways to maintain trust and safety. Establish legal and ethical review processes to navigate liability concerns and align deployments with evidence-based medicine principles.

Illustration of challenges like silos, bias, regulation, and strategies to mitigate each
Exploring Advanced Techniques for Augmented Intelligence in Medicine
Advanced techniques combine generative models, multimodal fusion, and reinforcement learning to support complex clinical tasks such as personalized treatment planning and dynamic triage. Integrating language models with imaging pipelines and structured data enables systems that can summarize patient histories, propose differential diagnoses, and highlight evidence grounded in cited literature. Use transformer model architectures for sequence-to-sequence tasks, and apply deep-learning applications for imaging and physiological signal analysis. Teams should validate models via prospective trials and external datasets, report findings to official websites and peer-reviewed journals, and ensure HTTPS-secured APIs for deployment. These techniques demand careful attention to interpretability and clinician workflows to maximize adoption and reduce false discoveries.

Visualization of multimodal AI combining imaging, notes, and labs to produce clinical recommendations
Expert Tips for Maximizing AI in Clinical Settings
Experts recommend starting with high-value, low-risk use cases, investing in clinical champion roles, and ensuring explainability and monitoring to sustain trust. Incorporate continuous feedback loops where clinicians annotate model errors, enabling iterative retraining on domain-specific datasets and improving performance on biomedical tasks. Prioritize interoperability through standardized APIs and HTTPS for secure communications, and align evaluation metrics with patient-centered outcomes like reduced time-to-treatment and improved patient satisfaction. Invest in education to upskill clinicians on model interpretation and human-AI collaboration, and publish results through the Journal of Medical Artificial Intelligence or JAMA Network for peer validation.
Checklist graphic showing expert recommendations: choose use case, train, validate, monitor, publish outcomes
Optimization Strategies for Reducing Physician Burnout with AI Tasks
Optimization strategies include automating routine documentation, triage prioritization, and administrative workflows to free clinician time for complex patient care and reduce burnout. Implement language models to draft notes and summarize patient portal messaging, while maintaining clinician review to ensure accuracy and alignment with clinical decision making. Monitor burnout metrics and clinician satisfaction before and after deployment, and adjust thresholds to balance sensitivity with false-positive rates. Use evidence-based medicine to justify automation, and track outcomes such as reduced after-hours charting and improved patient follow-up. Also, design systems that minimize interruptions and present clear rationale for recommendations to support clinician autonomy.
Graphic showing reduction in after-hours work and improved clinician satisfaction after AI automation
Impactful Applications of Generative Artificial Intelligence: Industry and Academic Insights
Generative artificial intelligence has catalyzed new research workflows and clinical tools, from accelerating literature review to generating synthetic datasets for augmentation while protecting privacy. Academic collaborations have produced promising results in diagnostics and patient triage, and industry partnerships drive scalable deployments that emphasize ROI and workflow fit. Case studies show gains in documentation efficiency and triage accuracy, but also underscore the need for robust validation approaches and transparent reporting in peer-reviewed venues such as the Journal of Medical Artificial Intelligence. Institutions should balance innovation with governance, invest in domain-specific datasets, and ensure HTTPS-secured endpoints for any third-party integrations. For operational guidance on aligning enterprise objectives and ROI, review practical frameworks from industry leaders like enterprise ROI and AI strategies to balance adoption speed with measurable value.
Collage showing academic papers, enterprise dashboards, and clinician-AI collaboration in clinical research settings
Revealing Transformative Case Studies: AI in Health Care Success Stories
Analyzing case studies reveals common success factors: strong clinician involvement, iterative validation, and measurable operational KPIs such as reduced wait times or improved diagnostic accuracy. Success stories include deep-learning applications in radiology that improved lesion detection, language models that reduced documentation time, and predictive models that improved patient triage and follow-up adherence. These deployments emphasize the importance of domain-specific datasets and prospective evaluation to ensure real-world performance. Reporting outcomes through official websites and peer-reviewed journals promotes transparency and fosters broader adoption across healthcare systems. Practitioners should emulate the governance, monitoring, and clinician training components demonstrated in successful pilots.

Case study montage showing radiology improvement, documentation reduction, and predictive triage impact
Inspiring Success Stories of AI-powered Tools in Medicine
Inspiring deployments combine clinical relevance with rigorous evaluation: examples include oncology tools detecting microcalcifications, AI-assisted ECG interpretation reducing time-to-intervention, and language models that support discharge summaries. These projects prioritized external validation, clinician feedback loops, and monitoring to ensure sustained performance. Metrics reported often include improved diagnostics, patient triage efficiency, and clinician time savings, with results published in venues like JAMA Network to validate impact. Teams should document implementation steps, challenges, and lessons learned to help other institutions replicate success while adhering to evidence-based medicine practices.
Collage of success story snapshots: oncology detection, ECG analysis, and clinician workflow improvements
In-Depth Analysis of Artificial Intelligence Applications in Clinic Practice
Real-world deployments teach that governance, clinician engagement, and continuous monitoring are non-negotiable; neglecting any of these leads to stalled adoption or unsafe recommendations. Teams must plan for data drift, schedule retraining on new domain-specific datasets, and run ongoing bias audits. Integrating feedback mechanisms where clinicians can flag erroneous outputs helps refine models and improve trust. Transparent documentation, publication of evaluation results, and alignment with evidence-based medicine support broader acceptance. Additionally, organizations must prepare for organizational change, train staff, and measure both clinical and operational metrics to prove value.
Graphic displaying lessons learned: governance, retraining, audits, and clinician feedback cycles
Critical Roles of AI-powered Tools in Diagnosis
Emerging developments include multimodal models, improved generative artificial intelligence capable of grounded clinical reasoning, and tighter integration of machine learning with personalized medicine to support precision medicine and longitudinal care. Advances in transformer model architectures and language models will enable richer summarization and hypothesis generation for clinicians, but will require novel validation approaches and regulatory frameworks. There is growing interest in using AI for Biological Age estimations, predictive modeling for cancer survivorship, and improving patient triage through real-time analytics. Research funding such as Google PhD Fellowship programs and collaborative initiatives are accelerating impactful research, while journals like JMAI track emerging metrics like JMAI CiteScore 2.1 to assess field impact.
Futuristic graphic showing multimodal AI, personalized treatment pathways, and longitudinal patient monitoring
Identifying Important Factors for Successful AI Integration
The AI taxonomy will evolve to emphasize hybrid human-AI workflows, regulatory-ready validation categories, and task-specific benchmarks for medical AI to ensure safety and efficacy. Transformer model architectures, generative artificial intelligence, and specialized neural networks will be categorized by risk, explainability, and intended clinical use, guiding procurement and clinical adoption. Future taxonomy updates should incorporate performance on domain-specific datasets and include criteria for interoperability, HTTPS security, and continuous monitoring. This evolution will help clinicians, regulators, and vendors align around standards that support evidence-based medicine and accelerate responsible innovation.
Diagram projecting taxonomy evolution with categories for risk, explainability, and clinical use cases
In-Depth Analysis of Artificial Intelligence Applications in Clinic Practice
Over the next decade, expect deeper integration of AI into routine care, with AI-assisted diagnostics, automated documentation, and systems that personalize care pathways using patient-specific data to enable precision medicine. Advances in generative AI and language models will streamline research synthesis, accelerate clinical trial design, and support clinical decision making, but success will hinge on robust validation approaches, clinician training, and governance frameworks. Anticipate an expansion of interoperable, HTTPS-secured APIs and broader public reporting through official websites and peer-reviewed venues to drive transparency. Strategic planning should include investment in domain-specific datasets, clinician education, and monitoring systems to ensure sustained impact.
Timeline graphic predicting milestones in AI adoption, regulation, and clinical integration over next decade
Charting the Path Forward: Future Possibilities for Artificial Intelligence in Medicine Program
Charting a path forward requires translating insights into operational plans that prioritize patient safety, clinician engagement, and measurable outcomes such as improved diagnostics, precision medicine delivery, and reduced administrative burden. Develop a phased roadmap with pilots focused on high-value use cases, define validation approaches, and commit to publishing results in peer-reviewed outlets to support evidence-based medicine. Invest in domain-specific datasets, secure HTTPS infrastructure, and cross-functional teams to shepherd projects from prototype to scale. Emphasize training for medical students, primary care physicians, and specialists to foster adoption and maintain human oversight for clinical decision making. Lastly, align governance with organizational change management to embed AI solutions sustainably.

Strategic roadmap showing pilots, validation, scaling, education, and governance steps for AI programs
Recapping the Core Insights: Summary of Key Points in AI in Health Care
Key insights include the necessity of rigorous validation approaches, clinician engagement, and robust governance to realize benefits from Artificial intelligence and machine learning. Evidence-based medicine should guide deployment decisions, and organizations must prioritize HTTPS-secured data exchange, domain-specific datasets, and prospective evaluation to ensure safety and generalizability. Practical outcomes include improved diagnostics, streamlined documentation, and enhanced patient triage, while sustaining benefits requires monitoring, retraining, and transparent reporting. Interdisciplinary teams and clinician champions are essential to translate technical capabilities into clinical value and reduce physician burnout through thoughtful automation.

Summary infographic highlighting validation, governance, clinician engagement, and measurable outcomes
Concluding Thoughts on the Augmented Intelligence Revolution and Physician Sentiments
Physician sentiments reflect cautious optimism: clinicians value tools that save time and improve accuracy but demand transparency, interpretability, and clear accountability frameworks. Successful augmented intelligence deployments prioritize clinician control, integrate into workflows with minimal friction, and demonstrate measurable improvements in patient care and clinician workload. Education, peer-reviewed evidence, and early success stories drive confidence, while governance and continuous validation protect patient safety. Organizations should actively solicit clinician feedback and measure sentiment changes as part of adoption metrics to ensure sustained trust and utility in clinical settings.

Image showing clinician focus groups providing feedback on AI tools and sentiment metrics
Igniting Action: Your Next Steps in Understanding AI Solutions and Medical Artificial Intelligence
To take action, organizations should identify high-impact use cases, appoint clinical champions, and design pilot studies with clear KPIs tied to patient care and operational efficiency. Start small with focused trials that leverage domain-specific datasets and apply rigorous validation approaches, then iterate based on clinician feedback and monitoring outcomes. Secure HTTPS connections and ensure vendor transparency, and engage legal and compliance early to mitigate risk. Educate staff on interpreting AI outputs and incorporate mechanisms to measure changes in patient triage, documentation burden, and diagnostics. Publish pilot outcomes to contribute to evidence-based medicine and inform broader adoption across the health care ecosystem.

Action checklist showing define use case, assemble team, secure data, pilot, evaluate, publish results
Pathways to Progress: Essential Next Steps for AI in Clinic Practice
Essential next steps include building interdisciplinary teams, investing in labeled data, and establishing monitoring and retraining workflows to maintain model performance. Prioritize interoperable solutions with HTTPS-secured APIs and identify measurable success criteria such as reductions in after-hours work, improved triage efficiency, and better diagnostic accuracy. Engage clinicians early to co-design interfaces and escalation protocols, conduct prospective validation, and align projects with organizational strategy and ROI goals. Document lessons learned and share results in peer-reviewed forums to support community learning and accelerate responsible adoption.

Pathway diagram showing team formation, data curation, pilot execution, and scaling with KPI tracking
Expanding Your Knowledge: Access Options for Additional Information and JAMA Resources
To deepen knowledge, consult peer-reviewed resources, official websites, and specialty journals including JAMA Network and the Journal of Medical Artificial Intelligence for evidence-based guidance, methodological standards, and case studies. Engage in targeted training programs for clinicians and data scientists that cover Natural Language Processing, transformer model architectures, and deep-learning applications. Participate in workshops, boot camps, and advocacy updates to stay current on regulatory and ethical standards and leverage community resources like Creative Commons Attribution datasets for research. Prioritize HTTPS-secured repositories and official publications to ensure reliable information as you scale AI initiatives in health care.
Resource library depiction showing journals, guidelines, training modules, and secure data repositories














