
Delving into the C-section epidemic reveals multifaceted drivers, including changes in maternal age, increased rates of obesity, and the prevalence of labor induction. Older maternal age and certain pre-existing conditions often lead to a higher likelihood of surgical intervention. Additionally, the widespread use of electronic fetal monitoring, while crucial for identifying distress, can sometimes lead to ambiguous readings that prompt a C-section. There’s also the 'once a C-section, always a C-section' mentality, which, though not always medically accurate, often influences subsequent birth choices. These elements, combined with a cultural shift towards scheduled deliveries, contribute significantly to the high number of C-sections performed annually, transforming what was once an emergency procedure into a routine option for many.
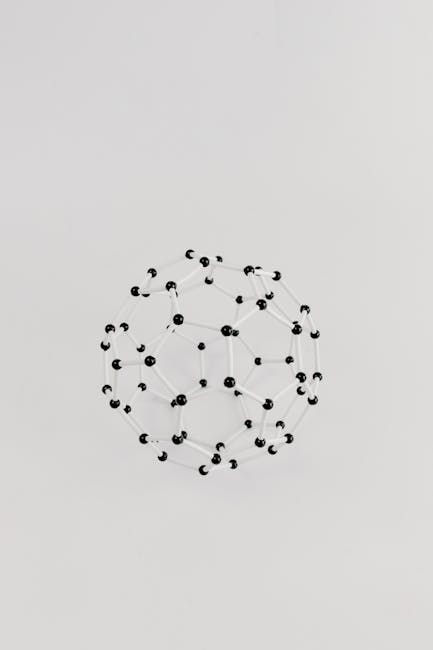
A flowchart illustrating the interconnected factors leading to an increase in Caesarean birth rates in modern obstetrical care
Critical Fetal Monitoring Protocols: Impact on C-Section Rate
Critical fetal monitoring protocols play an undeniable role in influencing the C-section rate. While intended to ensure the safety of both mother and baby, the interpretation of fetal heart rate patterns can be complex and sometimes lead to over-intervention. Continuous monitoring, particularly in low-risk pregnancies, might detect transient decelerations that are not indicative of true fetal distress but can trigger a cascade of interventions, culminating in a C-section. The pressure on healthcare providers to avoid any adverse outcomes also contributes to a lower threshold for surgical delivery. Therefore, refining guidelines and enhancing training for interpreting fetal monitoring data are crucial steps in reducing unnecessary C-sections, ensuring that interventions are truly medically necessary.

An illustration of a fetal monitoring device showing various readouts and a medical professional interpreting the data
Analyzing the C-Section Landscape: Beyond Superficial Discussions
Moving beyond superficial discussions about C-sections requires a deeper analysis of systemic issues within maternity care. The landscape is shaped by the availability of resources, insurance policies, and prevailing medical training. For example, some hospitals might have higher rates due to staffing models or a lack of access to alternative birthing methods. The focus often remains on individual patient choice, but the broader environment where childbirth occurs significantly impacts outcomes. Investigating how different models of obstetrical care influence C-sections alarming numbers can provide invaluable insights for policymakers and healthcare administrators seeking to improve maternal health. This necessitates a holistic view that considers the entire spectrum of factors influencing a woman's birth experience.

A panoramic view of a modern maternity ward, showcasing various care options and medical equipment in use
Crucial Elements Driving the High C-Section Rate in the United States
Several crucial elements drive the persistently high C-section rate in the United States. These include a higher rate of labor induction, often leading to more interventions, and a lack of access to midwifery care or birthing centers that prioritize natural childbirth. The medical-legal environment also creates a punitive element, pushing practitioners towards C-sections to mitigate perceived risks of litigation. Moreover, the cultural normalization of surgical delivery, coupled with a decline in vaginal birth after C-section (VBAC) attempts, perpetuates the cycle. Addressing these elements requires a multi-pronged strategy that encourages evidence-based practices, supports shared decision-making between patients and providers, and explores alternative care models to reduce the incidence of medically unnecessary C-sections.
A conceptual diagram illustrating the various systemic pressures contributing to the elevated C-section rate in the US healthcare system
The C-Section Conundrum: What News IS Driving This Medical Trend?
The C-section conundrum is a complex medical trend driven by evolving clinical guidelines, technological advancements, and shifts in societal perceptions of childbirth. News and medical publications frequently report on new research regarding optimal timing for C-sections, management of breech position, and guidelines for managing high-risk pregnancies, all of which influence obstetric practice. The increasing focus on personalized medicine also means that individual patient factors are being weighed more heavily. Furthermore, public awareness campaigns and discussions around maternal mortality and morbidity can influence both patient and provider decisions, sometimes leading to a more conservative approach favoring surgical delivery. This ongoing dialogue in the medical community and public sphere constantly reshapes the narrative around C-sections, contributing to their current prevalence.
A collage of recent medical news headlines and research papers discussing trends and controversies surrounding C-section rates
Decoding the Procedure & Recovery: A Comprehensive Guide to C-Section Care
Decoding the C-section procedure and recovery process is crucial for expectant mothers and their families. A C-section involves an incision through the mother's abdomen and uterus incision to deliver the baby. While a planned C-section allows for preparation, an emergency surgical delivery can be more challenging. Post-operatively, managing pain, promoting wound healing, and understanding the recovery time are paramount. This comprehensive guide helps demystify the process, addressing common concerns about mobility, breastfeeding, and emotional well-being after a Caesarean birth. Adequate rest, proper nutrition, and gentle activity are key to a smooth recovery. Understanding what to expect can significantly ease the anxieties associated with this major abdominal muscle surgery.
A diagram illustrating the layers of incision during a C-section procedure, with labels for clarity
Step-by-Step C-Section Process: Navigating Before Surgery & Post-Operative Care
Navigating the step-by-step C-section process, both before surgery and during post-operative care, requires clear communication and preparation. Before surgery, patients undergo assessments, receive anesthesia, and are prepped, often including an abdominal cleanse. The procedure itself typically takes less than an hour, followed by immediate skin-to-skin contact with the baby if possible. Post-operative care focuses on pain management, monitoring for complications, and encouraging early mobilization. Patients are usually encouraged to walk within 24 hours to prevent blood clots. Comprehensive discharge instructions, including wound care, activity restrictions, and signs of infection, are vital for a safe recovery at home.

A timeline graphic outlining the key stages of a C-section, from pre-op preparation to initial post-operative recovery
Analyzing the C-Section Landscape: Beyond Superficial Discussions
Revolutionary techniques are continually optimizing the C-section procedure and recovery, aiming to enhance patient experience and outcomes. These innovations include enhanced recovery after surgery (ERAS) protocols, which involve multimodal pain management, early oral intake, and early ambulation to accelerate healing. New suture techniques and wound closure methods are also minimizing scar visibility and improving comfort. Furthermore, advancements in anesthesia provide better pain control with fewer side effects. The goal is to transform the C-section from a highly invasive event into a more patient-centered experience, focusing on minimizing discomfort and facilitating a quicker return to normal activities, thereby reducing the overall recovery time.
An illustration demonstrating advanced surgical techniques used in modern C-sections for improved patient outcomes
Crucial Elements Driving the High C-Section Rate in the United States
Achieving a smoother procedure and recovery after a C-section involves a combination of preparation and adherence to expert tips. Prior to the surgery, discuss pain management options with your medical team and understand the recovery timeline. Post-procedure, focus on gentle movement, such as short walks, to promote circulation and prevent complications like blood clots. Utilize pillows for abdominal support when coughing or laughing, and ensure adequate rest. Engaging in early skin-to-skin contact with your baby can also aid bonding and recovery. Remember to hydrate well and consume nutrient-dense foods to support healing. Proper self-care and following medical advice are paramount for a positive outcome after this surgical delivery.
A mother holding her newborn baby in a hospital bed, emphasizing comfort and early bonding after a C-section
Global Insights & Future Horizons: C-sections, Driver's Licenses, and Israel's Military Draft
Exploring global insights provides a broader perspective on issues like C-sections, driver's licenses, and even societal dynamics such as Israel's military draft. While seemingly disparate, these topics intersect in ways that highlight advancements in technology, policy challenges, and the evolution of social norms. The global variation in C-section rates, for example, offers lessons for countries struggling with high numbers, demonstrating that cultural and healthcare system differences play a significant role. Similarly, the ongoing discussions around digital driver's licenses underscore a global move towards digital identity and streamlined administrative processes. Examining these diverse topics allows for a comprehensive understanding of interconnected global trends and future horizons in public policy and healthcare, emphasizing a holistic world view.

A world map highlighting different C-section rates globally, alongside icons representing digital driver's licenses and military service
Comparing Healthcare Outcomes: C-sections in the United States vs. Chinese Mothers
Comparing healthcare outcomes, specifically C-sections, between the United States and Chinese mothers reveals intriguing differences and similarities. Historically, China has faced exceptionally high C-section rates, driven by factors like fear of labor pain, one-child policy implications (desire for a 'perfect' baby), and patient preference for convenience. While the US also struggles with high rates, the drivers often include defensive medicine and maternal age. Both countries are now actively working to reduce unnecessary surgical deliveries, implementing new guidelines and promoting natural childbirth. The lessons learned from China's efforts to lower its C-sections alarming numbers can provide valuable insights for improving maternity care and reducing the C-section rate in the United States, fostering a more evidence-based approach to childbirth for American babies.
A comparative chart showing C-section rate trends in the United States and China over the past decade, with annotations
Success Stories: Reducing the C-Section Rate Through Innovative Fetal Monitoring
Several success stories demonstrate that reducing the C-section rate is achievable through innovative fetal monitoring and improved clinical practices. Hospitals that have implemented enhanced training for interpreting fetal monitoring data, coupled with decision-support tools, have seen significant reductions in unnecessary C-sections. For instance, some facilities have adopted intermittent monitoring for low-risk pregnancies, decreasing the likelihood of interventions. Others have focused on strengthening labor support systems, empowering pregnant women to progress naturally. These successes highlight the importance of a multi-pronged approach that combines technological advancements with patient-centered care, ultimately leading to better outcomes and a lower reliance on surgical delivery for American babies.
A hospital team celebrating a successful initiative to reduce C-section rates, with a banner highlighting their achievements
Lessons Learned: From Chinese Mothers to United States C-section Policy
Lessons learned from Chinese mothers in their efforts to reduce C-sections offer pertinent insights for United States C-section policy. China’s aggressive campaigns to promote vaginal birth, including public education and revised hospital policies, have demonstrated measurable success in lowering their previously soaring rates. Key takeaways include the importance of comprehensive prenatal education, empowering women with knowledge about childbirth options, and the critical role of government and healthcare institutions in shaping maternity care practices. Applying these insights to the US context could involve strengthening policies that support natural labor, expanding access to midwives and doulas, and creating incentive structures that reward lower C-sections alarming numbers when medically appropriate.
An image showing a traditional Chinese birth celebration alongside a modern American maternity ward, symbolizing cultural exchanges in healthcare policy
Analyzing the C-Section Landscape: Beyond Superficial Discussions
Beyond the current issue, future trends in procedure and recovery for C-sections point towards even less invasive techniques and highly personalized care. Research is ongoing into methods that minimize abdominal muscle disruption, potentially leading to faster healing and reduced pain. Innovations in biomaterials for wound closure could also revolutionize recovery, enhancing comfort and aesthetic outcomes. The integration of artificial intelligence and machine learning in predicting C-section necessity based on individual patient data promises more accurate risk assessments, further reducing medically unnecessary C-sections. This forward-looking approach aims to make the C-section a safer, more efficient, and more comfortable experience for mothers worldwide.
A futuristic rendering of a surgical suite with advanced robotic assistance for C-sections, highlighting innovation
Crucial Elements Driving the High C-Section Rate in the United States
Emerging developments highlight how digital driver's licenses could revolutionize the way healthcare data is managed and accessed, particularly in critical situations like C-sections. By securely linking digital ID cards with medical records, healthcare providers could swiftly access essential patient information, including allergies, pre-existing conditions, and birth history, even during emergency surgical delivery procedures. This streamlines patient identification and information exchange, particularly before surgery, reducing administrative burdens and potential errors. The secure, standardized nature of digital driver's licenses, often aligned with AAMVA guidelines and ISO standard specifications, offers a robust framework for improving patient safety and continuity of care across different medical settings.
A smartphone displaying a digital driver's license with medical data overlays, symbolizing secure data access in healthcare
Digital Driver's Licenses & Health Data: A New Frontier in Patient Safety & C-Section Care
Digital driver's licenses are poised to open a new frontier in patient safety and C-section care by offering a secure and efficient way to access critical health data. Imagine a scenario where, in an emergency, a healthcare provider could instantly verify a patient's identity and access their essential medical history, including previous C-sections, allergies, or chronic conditions, directly from their digital ID cards. This technological integration could significantly reduce delays and errors, particularly in urgent situations involving pregnant women. The standardized format of these digital credentials, often adhering to an ISO standard, ensures interoperability and security, making them a powerful tool for enhancing patient safety and streamlining administrative processes within maternity care settings.

A digital representation of a driver's license with integrated health symbols, demonstrating its potential for patient safety
Transforming Patient Experience: Before Surgery and Recovering from a C-section
Transforming the patient experience, both before surgery and during the process of recovering from a C-section, is paramount for modern healthcare. Digital driver's licenses could play a vital role here by enabling seamless check-ins and immediate access to pre-operative instructions and personalized recovery plans. This would alleviate stress and ensure patients are well-informed. Furthermore, secure digital access to medical records could allow healthcare providers to tailor care more effectively, anticipating potential complications based on comprehensive patient history. This personalized approach to a C-section, from the initial consultation to post-operative follow-ups, would significantly enhance patient satisfaction and lead to better health outcomes, reducing the overall recovery time.
A patient interacting with a digital health portal on a tablet, illustrating improved pre-operative and post-operative experience
Analyzing the C-Section Landscape: Beyond Superficial Discussions
The essential role of Real ID in streamlining healthcare access, particularly for procedures like a C-section, cannot be overstated. By providing a federally compliant form of identification, Real ID cards facilitate quicker and more accurate patient registration across different healthcare facilities. This is crucial for verifying patient identity and ensuring that the correct medical records are accessed, minimizing the risk of medical errors. In emergency scenarios, the ability to quickly confirm a patient's identity and retrieve their history, especially regarding previous surgical delivery or any existing conditions, can be life-saving. The integration of Real ID principles with digital driver's licenses promises an even more efficient and secure system for healthcare access.
A close-up of a Real ID card, emphasizing its security features and federal compliance
Crucial Elements Driving the High C-Section Rate in the United States
Leveraging digital driver's licenses for improved patient identification involves several key concepts, central to modernizing healthcare delivery. These include secure digital authentication, interoperability across healthcare systems, and robust data privacy measures. By using cryptographic technologies, digital driver's licenses can provide irrefutable proof of identity, far surpassing traditional physical ID cards. This enhanced security is vital in preventing medical identity theft and ensuring that personal health information remains confidential. The potential for these digital credentials to seamlessly integrate with electronic health records (EHRs) and AAMVA standards means that patient identification during a C-section or any medical procedure becomes instant, accurate, and highly secure.

A graphic illustrating the secure digital authentication process of a digital driver's license in a healthcare context
Analyzing the Impact: Real ID's Influence on C-section Procedure & Recovery
Analyzing the impact of Real ID on the C-section procedure and recovery reveals tangible benefits for efficiency and patient safety. By standardizing identification, Real ID reduces delays in administrative processes, ensuring that patients can quickly access pre-operative consultations and that necessary medical records, including details of previous C-sections or any relevant health conditions, are retrieved without hindrance. This efficiency translates into smoother patient flow, better allocation of resources, and potentially shorter wait times before surgery. During recovery, accurate identification ensures that post-operative care instructions, prescriptions, and follow-up appointments are correctly assigned and communicated, minimizing errors and enhancing the overall quality of care for mothers recovering from a C-section.

A patient confidently presenting a Real ID at a hospital reception desk, symbolizing streamlined access to care
Critical Elements: Ensuring Seamless Information Exchange Before Surgery
Ensuring seamless information exchange before surgery is among the critical elements for optimizing the C-section procedure. Digital driver's licenses, integrated with healthcare systems, can facilitate this by providing a unified digital identity that instantly links to comprehensive patient records. This includes critical details like blood type, allergies, current medications, and any history of a previous surgical delivery. Such instantaneous access to information allows the surgical team to make informed decisions quickly, minimizing risks and customizing the approach for each patient. It also helps in preparing for potential complications and ensures that all necessary resources are ready in the operating rooms, making the entire process more efficient and safer for the pregnant women.

A medical team reviewing digital patient records on a screen before a C-section, emphasizing seamless information access
More On Companies & Innovation: The Lung Cancer Biomarkers Market in Healthcare
The North America Lung Cancer Biomarkers Market is experiencing rapid growth, fueled by significant advancements in personalized medicine and diagnostic tools. This burgeoning sector is crucial for enhancing the detection, prognosis, and treatment monitoring of lung cancer. Companies are continuously innovating to discover novel biomarkers that can lead to earlier detection, more accurate staging, and tailored therapeutic strategies. The focus is shifting towards minimally invasive diagnostic procedures, such as liquid biopsies, which offer less discomfort and quicker results than traditional tissue biopsies. The market's expansion is driven by the increasing incidence of lung cancer globally and the imperative for more effective, patient-specific healthcare solutions, making it a critical area of research and development.
A microscopic view of lung cancer cells with highlighted biomarkers, representing advancements in diagnostic tools
The Rise in Use: Advanced Techniques for Lung Cancer Biomarkers Market Growth
The rise in use of advanced techniques is a primary driver for the Lung Cancer Biomarkers Market growth. Innovations in genomics and proteomics, coupled with high-throughput screening methods, are enabling the identification of an ever-expanding array of biomarkers. These techniques allow for a deeper understanding of lung cancer at a molecular level, facilitating the development of targeted therapies. Furthermore, the increasing adoption of personalized medicine approaches necessitates sophisticated biomarker analysis to match patients with the most effective treatments. This continuous evolution of diagnostic capabilities not only improves patient outcomes but also fuels the market expansion by creating demand for cutting-edge biomarker tests and related services.

An infographic illustrating the various advanced techniques used in lung cancer biomarker discovery and analysis
Step-by-Step Process: Navigating the Lung Cancer Biomarkers Market Landscape
Navigating the Lung Cancer Biomarkers Market landscape involves a step-by-step process of research, development, and commercialization. Initially, this involves extensive scientific research to identify potential biomarkers from patient samples. This is followed by rigorous validation through clinical trials to confirm their efficacy and reliability. Once validated, these biomarkers are integrated into diagnostic Test Kit products, which then undergo regulatory approval processes. Commercialization involves strategic marketing, distribution, and partnerships with healthcare providers and pharmaceutical companies. Understanding this intricate journey is crucial for companies looking to penetrate or expand their presence in this rapidly evolving sector, ensuring their innovations effectively reach patients needing lung cancer detection and treatment.
A detailed flowchart illustrating the journey of a lung cancer biomarker from discovery to market launch
Common Challenges: Market Size Expansion and Competitive Landscape Analysis

































